What is Menopause?
Menopause is a natural biological process that signifies the end of a woman’s reproductive years. It typically occurs during the late 40s to early 50s, with the average age of onset being around 51 in many populations. Menopause is defined as having occurred after a woman has gone 12 consecutive months without a menstrual period. This stage results from a decrease in the production of hormones such as estrogen and progesterone, which play critical roles in regulating the menstrual cycle.
The transition to menopause is characterized by several stages. The first stage is known as perimenopause, which can start several years before menopause itself. During perimenopause, a woman may experience irregular menstrual cycles, fluctuating hormone levels, and a variety of symptoms such as hot flashes, mood changes, and sleep disturbances. This transitional phase may last anywhere from a few months to a decade, depending on the individual. Following perimenopause, a woman enters menopause, marked by the completion of her final menstrual period. The final stage is postmenopause, which lasts for the rest of a woman’s life and brings about long-term hormonal changes.
Biologically, menopause occurs as the ovaries gradually lose their ability to produce eggs, leading to a decrease in estrogen and progesterone levels. These hormonal shifts can bring about various physical and emotional symptoms, including changes in libido, weight fluctuations, and hot flashes. Understanding menopause is crucial for women as they navigate these changes, which can have significant implications for both their physical health and well-being.
Common Symptoms of Menopause
Menopause is a significant transition in a woman’s life, marked by various physical and emotional symptoms that can be quite impactful. One of the most commonly reported symptoms is hot flashes, which are sudden sensations of heat often accompanied by sweating and a rapid heartbeat. These episodes can occur during the day or night, leading to disruptions in daily activities and sleep patterns. Hot flashes can vary in intensity and duration, often becoming a defining characteristic of this hormonal change.
Another prevalent symptom of menopause is mood swings. As hormone levels fluctuate, many women experience increased irritability, sadness, or anxiety, which may lead to difficulties in maintaining optimal mental health. These emotional changes can be exacerbated by sleep disturbances caused by night sweats, further complicating the transition into menopause.
Fatigue is also a frequently reported symptom. Many women find themselves feeling unusually tired, even after a full night’s sleep. This can be attributed to hormonal imbalances as well as sleep disruptions caused by menopause-related symptoms such as hot flashes and night sweats. The combination of hormonal shifts and inadequate rest can significantly affect one’s energy levels and overall quality of life.
Moreover, changes in menstrual patterns are often noticeable during the menopause transition. Women may experience irregular periods, including variations in flow intensity and cycle length. This fluctuation in menstrual cycles can lead to confusion and concern, prompting many to seek information about this natural stage of life.
Understanding these common symptoms is crucial for women navigating menopause. Recognizing these experiences can facilitate better communication with healthcare providers, ensuring support and strategies for managing the transition effectively.
What Are Night Sweats?
Night sweats, also known as sleep hyperhidrosis, are characterized by excessive sweating during the night that can drench sleepwear and bedding, even in a comfortably cool setting. Unlike regular sweating, which can occur due to a variety of factors such as exercise, heat, or stress, night sweats are specifically tied to hormonal changes in the body. They are particularly prevalent during the menopausal transition, a period marked by fluctuating estrogen levels that contribute to various physical symptoms.
During menopause, the body experiences a significant hormonal imbalance as the ovaries gradually decrease their production of estrogen. This decrease can disrupt the body’s ability to regulate temperature effectively, often triggering episodes of night sweats. These episodes may present as sudden feelings of intense heat and typically occur during the night, disrupting sleep and leading to feelings of discomfort upon waking. Women experiencing night sweats may also encounter accompanying symptoms like chills, which occur as the body attempts to cool down after the sweating episode.
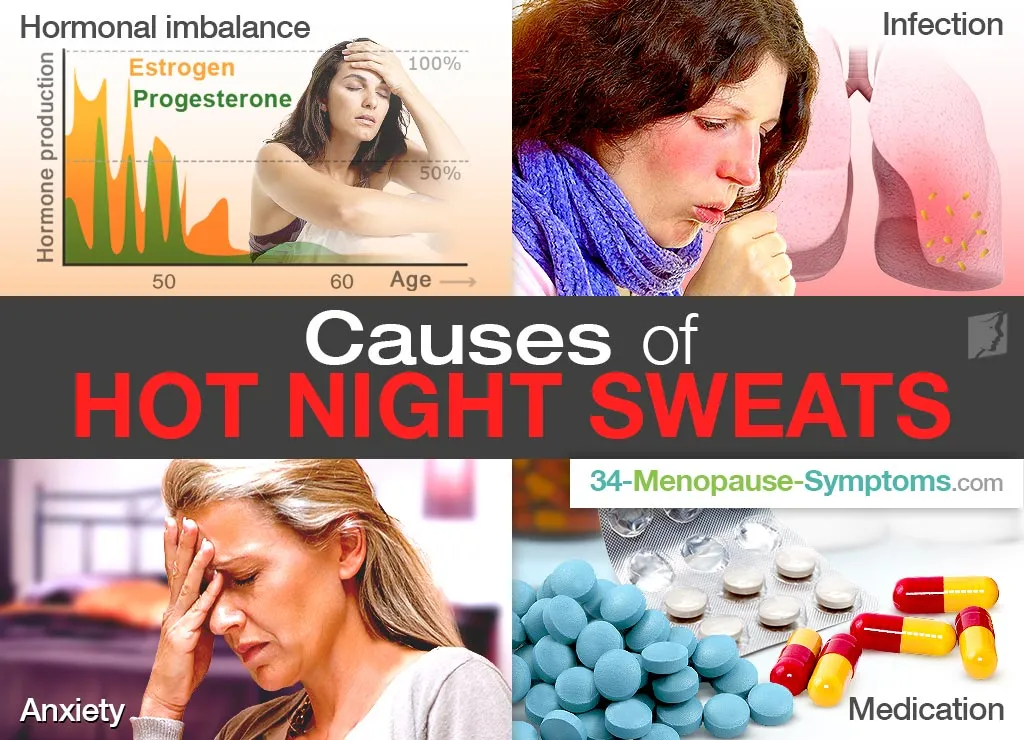
It is important to differentiate night sweats from other causes of nighttime perspiration, such as infections, medication side effects, or underlying health conditions. While occasional episodes of sweating during sleep may be deemed normal, frequent occurrences warrant further investigation, especially when they significantly affect quality of life. Recognizing the relationship between night sweats and menopause is essential for effectively managing symptoms. Understanding that these night sweats are a natural aspect of hormonal changes can help women navigate this challenging phase with more awareness and preparedness.
The Science Behind Night Sweats
Night sweats are a common symptom experienced by many women during menopause, largely attributed to hormonal fluctuations. The primary hormone involved in this process is estrogen, which plays a critical role in regulating the body’s temperature control system. As women approach menopause, estrogen levels decline, leading to an imbalance in hormone levels. This imbalance can significantly impact the hypothalamus, the part of the brain responsible for maintaining homeostasis, including temperature regulation.
The hypothalamus is sensitive to changes in hormone levels, and when estrogen decreases, it may misinterpret the body’s temperature. As a result, it triggers a cascade of responses that can lead to feelings of overheating. When the hypothalamus detects these changes, it activates the autonomic nervous system, which causes the body to sweat excessively in an attempt to cool down. This reaction is often termed a thermoregulatory disturbance and is a primary contributor to episodes of night sweats.
In addition to estrogen, other hormones such as progesterone also play a role in thermal regulation. As the levels of these hormones fluctuate during menopause, it can lead to increased thermoregulatory instability, exacerbating the condition. Furthermore, psychological factors, including stress and anxiety, can intensify the severity of night sweats, creating a cycle that compounds the experience of excessive sweating during sleep.
Understanding the science behind night sweats not only sheds light on the physiological changes that occur during menopause but also helps women navigate their experiences. By recognizing the factors contributing to these symptoms, women can explore various management strategies, including lifestyle modifications, dietary changes, and consulting healthcare professionals for appropriate treatment options. Ultimately, a better understanding of night sweats can empower women as they transition through this significant phase of life.
Impact of Night Sweats on Quality of Life
Night sweats are a common symptom experienced by many women during menopause, and their impact on quality of life can be profound. These episodes can lead to significant sleep disruption, preventing individuals from achieving the restorative benefits of a full night’s sleep. Inadequate sleep often results in daytime fatigue, decreased concentration, and reduced productivity, making it difficult to function effectively in daily tasks. Over time, the compounding effects of this disrupted sleep may contribute to chronic health concerns, including cardiovascular issues and weakened immune response.
The emotional ramifications of night sweats are equally substantial. Many women report feelings of embarrassment and discomfort associated with these sudden sweats, which can affect their self-esteem and body image. This emotional toll can lead to heightened anxiety, depression, and social withdrawal. Fear of potential night sweats can cause individuals to avoid situations where they may feel exposed or uncomfortable, such as social gatherings or intimate relationships, leading to feelings of isolation. The cumulative psychological impact can detract from one’s overall quality of life and interpersonal relationships.
Furthermore, the implications extend beyond the individual experience, potentially straining relationships with family and friends. Partners may struggle to understand the challenges posed by night sweats, leading to a disconnect in communication. It is essential for those experiencing this symptom to seek supportive networks and open dialogue with loved ones to foster understanding and empathy during this transitional period. Addressing night sweats is crucial not only for physical comfort but also for emotional well-being and maintaining healthy social interactions.
Effectively managing night sweats can enhance overall quality of life, allowing individuals to navigate menopause with greater ease and satisfaction. By recognizing and addressing this symptom, women can reclaim control over their daily experiences.
Body Changes During Menopause
Menopause marks a significant transition in a woman’s life, characterized by a range of physical changes resulting from hormonal fluctuations. As estrogen and progesterone levels decline, various bodily transformations can occur, impacting numerous systems within the body. One of the most commonly reported changes is weight gain, often localized in the abdominal area. Research indicates that women may experience an increase in body fat while simultaneously losing muscle mass during this phase of life. According to a study published in the Journal of Women’s Health, many women report an average weight gain of 5 to 10 pounds during the menopausal transition.
Another notable change is related to skin health. Many women find that their skin becomes thinner and less elastic due to decreased estrogen levels. This can lead to increased dryness, wrinkles, and an overall dull complexion. A survey conducted by the North American Menopause Society revealed that nearly 30% of women reported significant skin changes during menopause, with testimonials often highlighting the emotional impact these changes can have on self-esteem.
Altered body composition is also a key aspect of this transition. Women may notice changes in their body shape as fat distribution shifts, leading to an increase in visceral fat and a loss of subcutaneous fat. This can elevate the risk of various health issues, including cardiovascular disease and diabetes. It is essential to recognize that experiences of menopause can vary widely. Factors such as genetics, lifestyle, and existing health conditions contribute to how women perceive and manage these changes.
Understanding these body changes is crucial as it empowers women to seek appropriate strategies for managing their health during this transition. Increased awareness allows for a proactive approach that includes dietary modifications, regular exercise, and seeking guidance from healthcare professionals to help mitigate unwanted effects associated with menopause.
Coping Strategies for Night Sweats
Night sweats, a common symptom experienced during menopause, can significantly impact sleep quality and overall well-being. Implementing effective coping strategies can help manage these episodes more successfully. One of the first approaches is to consider lifestyle modifications. Diet plays a crucial role; it is advisable to avoid spicy foods, caffeine, and alcohol, as they can trigger or exacerbate hot flashes and night sweats. Instead, incorporating a balanced diet rich in fruits, vegetables, whole grains, and healthy fats is recommended to support overall health during this transitional phase.
Regular exercise can also be beneficial. Engaging in moderate physical activity, such as walking, swimming, or yoga, not only helps regulate body temperature but also improves mood and promotes better sleep. Experts suggest reiterating the importance of maintaining a consistent schedule for exercise while avoiding vigorous workouts close to bedtime.
Environmental adjustments can make a significant difference in managing night sweats. Optimal bedroom temperature, ideally between 60°F and 67°F, can aid in cooler sleep. Utilizing breathable, moisture-wicking bed linens and pajamas can help wick away moisture, providing greater comfort during the night. Additionally, having a fan or air conditioning can facilitate a cooler sleeping environment and reduce the likelihood of sweating episodes.
Good sleep hygiene is another important factor in managing night sweats. Establishing a relaxing bedtime routine, such as reading or practicing mindfulness meditation, can help prepare the body for restful sleep. Limiting screen time before bed and creating a calming environment can also enhance sleep quality.
Furthermore, for those experiencing severe night sweats, consulting a healthcare provider may be necessary. Medical treatments, including hormone replacement therapy and non-hormonal medications, can be effective in alleviating symptoms. Tailoring an individualized approach, combining lifestyle changes with professional medical advice, can greatly enhance the management of night sweats during menopause.
Navigating Emotional Changes
Menopause is a significant transition in a woman’s life, marked not only by physical changes but also by notable emotional and psychological impacts. The hormonal fluctuations that occur during this phase can lead to increased feelings of anxiety, irritability, and sadness. Night sweats, coupled with other bodily changes, can exacerbate these emotions, leaving many women feeling overwhelmed and isolated. Understanding these emotional shifts is crucial for effective navigation through this period.
Anxiety during menopause can manifest as persistent worry, restlessness, or difficulty concentrating. Women may find that previously manageable stressors become overwhelming, largely due to the physiological changes accompanying menopause. Furthermore, the unpredictability of night sweats can contribute to sleep disturbances, which significantly impact one’s emotional health. Sleep loss and discomfort can lead to a vicious cycle of heightened anxiety and mood fluctuations, emphasizing the importance of self-care and awareness of these changes.
Depression is another common emotional challenge faced during menopause. Feelings of sadness and low energy can seep into daily activities, affecting relationships and overall quality of life. Women should recognize that these feelings are valid and not uncommon. Seeking support during these times can be invaluable. Therapy can provide a safe space for individuals to express their feelings and concerns while developing coping strategies. In addition, support groups allow women to share experiences and find comfort in knowing they are not alone in their struggles. Conversations with friends and family can also foster a supportive environment, helping to alleviate feelings of isolation.
Ultimately, acknowledging and addressing the emotional changes during menopause is essential. Embracing support through therapy, support groups, or open discussions can assist in navigating this challenging phase of life, promoting emotional resilience and wellbeing.
When to Consult a Healthcare Provider
Menopause is a natural phase of life that can bring about various physical and emotional changes. While many women adapt to these transitions, there are instances when seeking medical advice becomes crucial. Women experiencing severe or persistent symptoms during menopause should consult a healthcare provider to discuss potential treatment options. Symptoms such as intense night sweats, significant mood swings, or persistent fatigue can greatly impact daily life and may require professional intervention.
Individualized treatment plans play a vital role in managing menopause symptoms effectively. Every woman’s experience is unique, influenced by personal health history, lifestyle, and specific symptoms. Consulting with a healthcare professional allows for a tailored approach, addressing individual needs while considering various therapeutic options. Healthcare providers can recommend hormonal therapies, lifestyle changes, or alternative treatments suited to a woman’s unique circumstances. This individualized care can enhance quality of life and provide relief from distressing symptoms.
Additionally, discussing personal health history with healthcare providers is essential in understanding how menopause may affect one’s overall health. Women should inform their doctors about previous medical conditions and any family history related to menopause or hormone-related issues. This information is critical in evaluating risks and determining the most appropriate treatment options. Moreover, involving healthcare providers in discussions about menopause-related symptoms fosters a supportive environment, promoting a comprehensive care strategy that encompasses both physical and emotional well-being.
Ultimately, it is important for women to recognize that while menopause is a natural transition, the accompanying symptoms can vary widely. Seeking medical advice at the appropriate time helps ensure that any concerning changes are addressed effectively, paving the way for a more manageable transition through menopause.